Background: The level of MRD before and after transplantation is related to inferior transplant outcomes, and post-hematopoietic stem cell transplantation measurable residual disease (post-HSCT MRD) has higher prognostic value in determining risk than pre-HSCT MRD. However, no work has been devoted to the risk factors for positive post-HSCT MRD in patients with ALL. This study evaluated the risk factors for post-HSCT MRD positivity in patients with acute lymphoblastic leukemia (ALL) who underwent allogeneic HSCT (allo-HSCT).
Methods: A total of 1683 ALL patients were enrolled. Cox proportional hazard regression models were built for time-to-event outcomes. Multivariate analysis was performed to determine independent influencing factors from the univariate analysis.
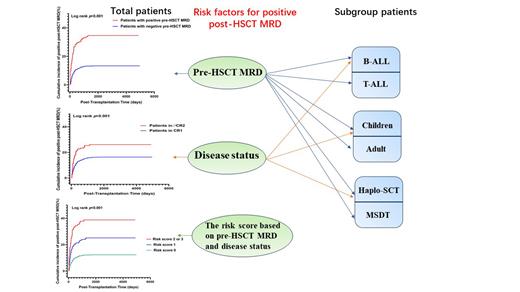
Results: Both in total patients and in T-ALL or B-ALL, pediatric or adult, HLA-matched sibling donor transplantation or haploidentical HSCT subgroups, positive pre-HSCT MRD was a risk factor for post-HSCT MRD positivity ( P < 0.001 for all). Disease status was also a risk factor for post-HSCT MRD positivity in all patients and in the B-ALL, pediatric, or haploidentical SCT subgroups ( P =0.003; P=0.035; P =0.003, respectively). A risk score for post-HSCT MRD positivity was developed using the variables pre-HSCT MRD and disease status. The cumulative incidence of post-HSCT MRD positivity was 12.3%, 25.1%, and 38.8% for subjects with scores of 0, 1, and 2-3, respectively ( P<0.001). Multivariate analysis confirmed the association of the risk score with the cumulative incidence of post-HSCT MRD positivity and relapse as well as LFS and OS.
Conclusion: Our results indicated that positive pre-MRD and disease status were two independent risk factors for post-HSCT MRD positivity in patients with ALL who underwent allogeneic HSCT.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal